Dr. Stallings here. I love to hate A1c. Give me sensor glucose data any day! We have 3 choices when it comes to measuring blood glucose control:
- Finger stick blood sugar checks
- HgbA1c
- Sensor glucose
Recent research has confirmed that sensor glucose is the most accurate out of the bunch. This is also my favorite way of measuring glucose control because of its details and accuracy. More on that in a moment…
Hemoglobin A1c is a 90 day average of your blood sugar levels. It reads as a percentage, such as 7.2%, and is measured using red blood cells (RBCs). It is measured as a percentage because we are essentially measuring what percent of the surface of the RBCs is covered with glucose molecules. The higher your blood sugar levels, the more glucose floats in your bloodstream; therefore, more glucose sticks to your RBCs. The lower your blood sugar, the fewer glucose molecules in your blood; not as many are there to stick to your RBCs. The higher percentage of glucose on the RBC reads as a higher A1c = your blood sugar levels are not as well controlled. If your A1c levels is lower (such as 6.1%), your blood sugar levels are lower, so there is less glucose to stick to the RBCs. Why do we check it every 90 days? That’s how long a RBC lives! We check A1c every 90 days to let the new batch of RBCs circulate in your bloodstream and collect the current level of glucose in your blood. If you started a new medication at your last visit, the med will have had 90 days to lower your serum (blood) glucose levels. There is less sugar in your blood to stick to the RBCs, so your A1c level should be lower.
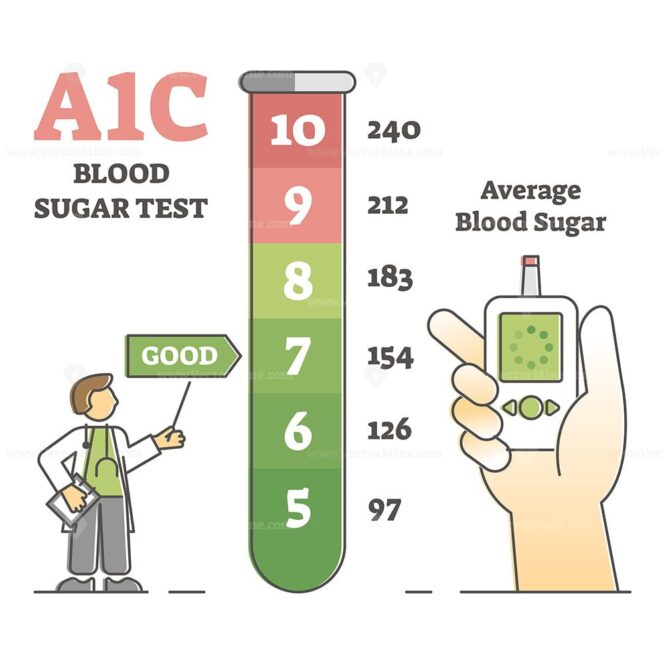
A1c is the gold standard on which we measure glucose and diabetes control. The American Diabetes Association recommends a goal of less than 7.0% for most diabetics. But this is a not a foolproof system. An A1c level of 7.0% is equal to a blood sugar level of 154 mg/dL. (Chart below.) But what it doesn’t tell us is when the sugars are high, when they’re low, how often they’re high or low, and most importantly, how high or how low the sugars get. An A1c level of 7.0% looks good on paper, but if your sugars are consistently dropping to 54 mg/dL overnight, but spiking to 254 mg/dL anytime you eat, these may average out to 154 mg/dL (or an A1c of 7.0%), but your blood sugars are far from being well controlled. However, A1c doesn’t give us any of this information. It is good for trending – is your level higher or lower at this visit than the last visit – but overall leaves us with more questions than answers in the form of solid glucose data.
Fingerstick blood sugars are something almost every diabetic is asked to do, but they have many of the same pitfalls as A1c. I will normally ask my patients to check their blood sugar first thing in the morning (fasting: nothing to eat or drink), and again in the evening before dinner or before bed. The fasting value is going to tell me about your overnight glucose control, whereas the evening value will tell me how well your sugars are controlled during the day (including meals). Once again, these levels can fluctuate based on what you ate and when you ate it. We can also use these levels for trending, and to determine if we need to concentrate more on improving your daytime or nighttime control.
But for my money, it’s sensor glucose all the way. First to clear up the reason that sensor and blood glucose values do not measure the same. They aren’t measured in the same fluid! Blood glucose is measured from a fingerstick and uses capillary blood. Sensor glucose has a small filament that remains just below the skin in the space between the blood vessels and the skin – called the interstial space. Sensor glucose therefore measures interstitial fluid. Glucose must first pass out of the blood stream, through the vessel wall, and into the interstitial fluid, so there will always be a lag between blood and sensor glucose. Sensor glucose can be 5-15 minutes behind blood glucose, and can be as many as 10-20 mg/dL apart from the blood glucose (or fingerstick) value. So then why is sensor glucose more accurate? Trending! When you test your blood sugar, you’re getting the reading for that one moment in time. Is your sugar rising, falling, or stable? We don’t know with a fingerstick alone. We certainly don’t know with a 90-day A1c. The sensor – also called continuous glucose monitoring, or CGM – is able to predict if your sugar is rising, falling, or remaining stable. It can also alert you if your sugar is going to be too high (usually over 240) or too low (usually below 70) within the next 30-60 minutes. A sensor report tells you and your healthcare provider precisely how high or low your sugars are, and when.
Why does this matter? For example, during your visit today, I ran your A1c and it came back at 7.1%. Not bad! Your average blood sugar is around 157 mg/dL, improved from 8.5% at your last visit. But we started insulin at your last visit, so I’m asking if you are having any low sugars (less than 90). You say no. Thankfully, we ordered a Dexcom sensor when we started you on insulin 3 months ago, so I pull up your Dexcom report. The estimated A1c (or GMI – glucose measurement index) on your Dexcom report is 6.4% and showing consistent overnight hypoglycemia (low blood sugar) into the 60s-70s. You’re a late riser, but your Dexcom is always between 100-130 when you wake up and check it. So what is the difference between the 90-day A1c of 7.1% and the 14-day estimate A1c of 6.4% on the Dexcom?
First, we can set our sensor reports to whatever length of time we want: 3 days, 14 days, 30 or 90 days, etc. This is true for the main 3 brands: Dexcom, Guardian, and Libre; my standard reports are set to 14 days. So what this means to me is that 3 months ago when your A1c was 8.5%, we decided to start you on insulin. In the ensuing 90 days, your blood sugars have come down a lot as you have continued to adjust your insulin according to the instructions you were given. During that 90 day cycle of RBCs (red blood cells), your A1c has dropped to a respectable 7.1%. But because it’s a 90 day average, and you have RBCs of different ages in your blood, we’re not getting the most accurate data. Because the sensor report is only reading the last 14 days – in interstitial fluid, not RBCs – we can see what your most recent control is. Therefore we know that you adjusted your insulin a bit too much, and it’s making your sugars drop overnight. So you agree to reduce your insulin dosage, but why are your sugars “normal” when you wake up? The sensor report will usually reveal a “bump” in sensor glucose between 3-5am, at which time your liver is kicking in and releasing some of its stored glucose (called glycogen) in an attempt to raise your blood sugar level closer to normal. This is what you are detecting on your monitor. By reducing your insulin dosage, you don’t have to worry about your fasting sugars getting too high; your liver will not have to release stored glycogen in response to the low sugars that were caused by too much insulin, so your sugars will remain stable – and “normal” – overnight.
Then why don’t we all have a sensor?! Say it louder for those in the back! But you can imagine my answer: insurance. Most commercial and federal plans will cover a sensor, but only if you are using insulin at least once a day. Some plans require the patient to inject insulin 3 times/day to cover a sensor and test your sugar at least four times/day. If your healthcare providers specializes in diabetes, the insurance pitfalls will be easier to navigate, and the landscape is changing on a weekly basis as more plans adopt sensors onto their formularies. Most of the companies, such as Freestyle Libre and Dexcom, have cash options for $75-85/month if your insurance company does not cover it, although this is still an investment.
Most plans cover a glucometer and test strips, but we often refer patients to Walmart Pharmacy for the ReliOn brand of meter and test strips for the most affordable option to monitor your blood sugar levels. Let us know if you have questions about your insurance coverage!