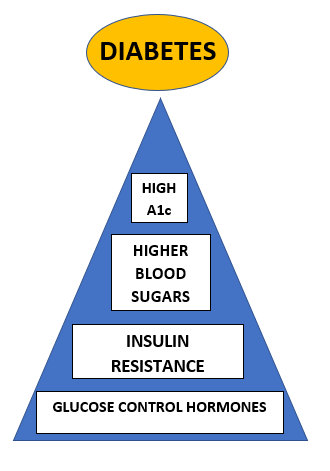
This is the most common question that people don’t ask. Most folks assume that because they have high blood sugar, they have diabetes, or vice versa – because they have diabetes, they have high blood sugars.
The reality of diabetes is that – at least for type 2 diabetics – diabetes results from a hormonal imbalance. Yes, genetics and lifestyle play a large role. We know the following genetic traits increase your risk of diabetes:
- Male
- Over age 45
- Ethnic groups such as African American, Asian, and Pacific Islanders
- Family history
You can’t change your genetics, so you can control your environment to reduce your risk of getting diabetes:
- Balanced diet
- Regular physical activity
- Healthy body weight

Type 1 diabetes is an autoimmune condition. You are born with antibodies in your blood – like little monsters – that attack the beta cells in your pancreas, mistakenly thinking they’re little invaders. The beta cells in your pancreas product the hormone insulin in response to rising serum (blood) glucose levels. However, the antibodies have attacked and killed enough beta cells that you cannot produce enough insulin to return your blood sugars levels to normal – therefore, they remain elevated. Over time, the antibodies destroy enough beta cells that a type 1 diabetic has a serum c-peptide (lab) level of zero, meaning their pancreas is no longer making any of its own natural insulin. There is no treatment for type 1 diabetes other than insulin (and a hormone injection called Symlin, not often used anymore).
Type 2 diabetes is different. It is not autoimmune and does not produce serum antibodies that attack the pancreatic beta cells. Over time, though, the beta cells are still destroyed which – coupled with insulin resistance – make your blood glucose levels rise. (More on insulin resistance in a moment.) How quickly or how slowly your beta cells are destroyed depends on the following characteristics:
- Blood glucose control – the higher your sugars, the harder your pancreas has to work, therefore overworking your beta cells as they keep trying to crank out more and more insulin in an attempt to return your blood sugars to normal; the beta cells burn out and die
- Diet – if you do not eat a balanced diet (portion control and moderation), your blood sugar levels remain elevated; see the bullet above for the rest of the story
- Medications – some of our older diabetes medications such as sulfonylureas (glipizide, glyburide, glimepiride) stimulate the beta cells in the pancreas to work harder to make more insulin, which is great in theory, but refer back to the first bullet to see how this makes diabetes progress over time
- Weight – the more weight you carry in your midsection, the more insulin resistant you are; I will explain insulin resistance next, but this is why glucose and diet control are so important
So what is insulin resistance? This has been a buzz word lately with products such as Golo hitting the market, promising to reduce insulin resistance and help people lose weight.
*Side note: I am often asked about Golo. I don’t have a problem with my patients using it, as long as the ingredients do not interact with their prescription medications. Golo is essentially an herbal supplement, and many herbs (such as St John’s Wort) will mess with common medications such as blood pressure meds and blood thinners. It works well for my patients while they use it, but there is not one case among my patients in which their diabetes and/or weight control has remained improved when they stopped using it. Something to consider. Now back to our regularly scheduled programming…
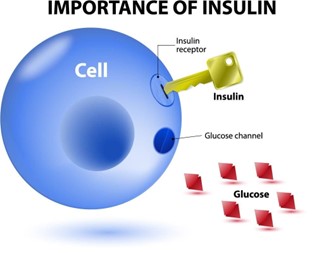
Insulin resistance occurs when the beta cells in the pancreas are steadily making insulin, but the body is unable to use it all. Insulin acts as the key to open our cells, let glucose into the cell, then the cell “closes the door” and converts the glucose into energy. Glucose is the fuel for our bodies like gas is the fuel for our cars. Our body uses the energy from glucose to first power our organs – brain, eyes, heart, kidneys, liver, etc. – and keep us alive. We get whatever is left over to power our day: wake up, walk to the bathroom, prepare meals, go to work. But when our hormones are out of whack, it’s harder for the insulin to bind to the cells to open the door. Therefore, more glucose stays in the blood stream instead of being converted into energy. This keeps blood glucose levels elevated, and energy levels low.
Many diabetics with uncontrolled blood glucose levels complain of being so tired that it’s difficult to function, especially toward the end of the day. The paragraph above is why. Then, throw abdominal fat and weight gain into the mix. Additional “fluff” around the midsection causes an increase in circulating free fatty acids (FFAs). These tiny fat globs prevent the insulin from being about to connect to our cells, making it even harder to metabolize glucose into energy. As you lose weight, your insulin sensitivity improves – reducing insulin resistance – and your blood sugar levels drop because the glucose is better able to enter the cells that have been unlocked by insulin. This returns your blood sugar and energy levels to normal, or close to it.
Great, so now what? A combination of lifestyle and medication is ideal to control insulin resistance:
- Diet: portion control, moderation, not deprivation
- Don’t count carbs alone; fat, fiber, protein, and calories are equally important
- Physical activity: notice I didn’t say exercise
- Exercise is great, but simply start by getting your body moving! Go for a walk, weed your garden, push mow your lawn, wash your car; get more active than you are now and build your activity level over time
- Stress: the biggest culprit of insulin resistance, stress must be considered and controlled
- Easier said than done, I know; but taking time for quiet reflection, meditation, reading a book, going for a walk, getting your nails done or having a massage are incredibly important to your overall health and well-being
- Medication: if meds are needed, work closely with your healthcare provider to use meds that do not put stress on your pancreas (such as glipizide and glimepiride listed above) and have additional health benefits (such as heart and kidney protection)
We’re happy to help! Contact Southside Diabetes to schedule an appointment and discuss your treatment plan with Dr. Stallings. In-person and telehealth visits are available!

