Pharmaco-whaaaa???
Pharmacogenomic testing lets us figure out which medications work with your DNA (or genetics) and which do not. In this case, we are comparing your DNA to any psychiatric mental health medication approved for use by the Food & Drug Administration (FDA) for use in the United States.
Okay cool … so why does that even matter?
The National Institute of Mental Health (NIMH) estimates 17.3 million American adults live with depression. That’s over 10% of the population. NIMH also estimates that 19.1% of adults in the US have had an anxiety disorder in the last 12 months, and 31.1% of US adults may experience anxiety at any time during their lives. And that doesn’t even include other mental health conditions such as post-traumatic stress disorder (PTSD), autism spectrum disorder, bipolar disorder, and schizophrenia, among others. More than 1 in 5 US adults live with a mental illness – totaling almost 58 million people in 2021. The Psychiatric Times estimates that mental health services totaled over $225 billion in 2019 and will cost the world $16 trillion USD by 2030.
So, what’s why it matters.
Mental health is one of the most prevalent yet least talked about conditions in all healthcare. People may feel shame and embarrassment about admitting their perceived “weaknesses” and may also fear being “labeled” as having a psychiatric or mental health condition. Primary care providers are most commonly the initial prescriber of mental health medications. Appropriate expectations on when to expect the medication to kick in, as well as potential side effects, are often not covered during the office visit due to time restrictions. Therefore, many patients take the medication for a week or two, feel no different, assume the medication isn’t working, and discontinue it. They are then even more reluctant to discuss their concerns with the healthcare provider(s) due to perceived “failure” of a medication – instead assuming there may be no hope for them, and they’re destined to “be like this” for the rest of the lives.
This is Dr. Stallings, and I’ve heard it all. I have heard those exact concerns and quotations from many of my patients. And yet the thing about mental health is it doesn’t just affect your emotions. I often have a great deal of trouble controlling blood glucose and HgbA1c levels psychiatric and mental health conditions are unidentified, untreated, mistreated, or undertreated. Patients often report extreme fatigue, lack of energy and motivation, worsening of their other health problems, and generally not caring about anything or anyone. Friends, family members, and coworkers notice too.
Mental health greatly diminishes your quality of life when not treated properly. This means we need to treat it quickly and correctly – the first time. Pharmacogenetic testing helps us do just that. Southside Diabetes has partnered with Tempus to offer personalized medication recommendations that are most likely to work with your DNA. Testing also tells us which medications do not work as well, and which medications should be avoided altogether. We will collect a saliva sample at the clinic and send it to the Tempus lab. We will receive your results electronically within 7-10 business days. At this time, your provider will make personalized recommendations for your medication management.
But does it work?
Yep. I suffered from postpartum depression after both my kids were born. My doctor put me on 2 different medications: Prozac (fluoxetine) and Lexapro (escitalopram). Neither worked to help my mood, but I gained over 20 pounds each time and entirely lost my libido. Being a new mom, I chalked it up to exhaustion. Fast-forward 5 years when I’m a working Nurse Practitioner, and I learned that these were side effects of these medications – also known as the SSRI (selective serotonin reuptake inhibitors) class. When I completed my genetic testing, the result came back as intolerant to all but one medication in the SSRI class. No wonder it didn’t work … makes sense.
In my 30s, I went back to my primary care provider and said I needed medication for anxiety. I didn’t have my Tempus results back yet, but I knew I didn’t want an SSRI. She instead prescribed Effexor XR (venlafaxine), an SNRI (serotonin norepinephrine reuptake inhibitor). Worked like a charm. I’ve now been on Effexor XR at various doses for over 4 years. My Tempus results indicate that both Effexor XR and the SNRI class are both genetically appropriate for me.
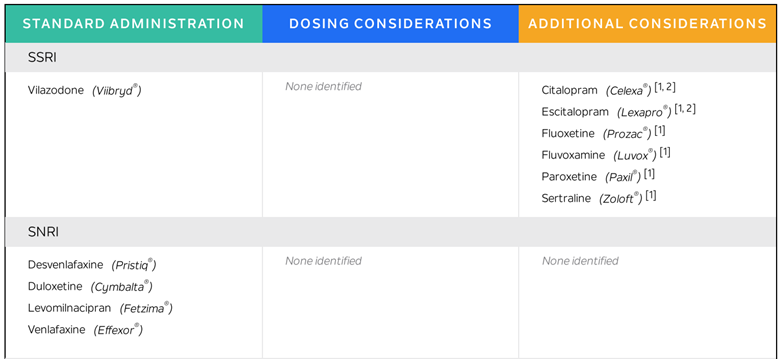
Here is a snapshot of my Tempus results:
I have since used this technology to help many of my patients who have tried and failed previous medications to find something better genetically matched to treat their symptoms. I also caution my patients about being realistic about when they will begin to feel differently after starting a new medication:
- 2-4 weeks to feel any effect
- 6-8 weeks to feel better
- 9-12 weeks to feel the full effect
When people know what to expect, they tend to hang in there with the medication for longer instead of becoming frustrated that the medication hasn’t changed their mood overnight. I also caution patients not to “cold turkey” or abruptly quit any mental health medications. Instead, call the clinic if you are experiencing side effects or want to wean up or down on your medication dosage.
Testing is 100% covered by Medicare and Medicaid. It may be fully or partially covered by Tricare and commercial plans. Tempus will contact you directly to discuss cost. The maximum out-of-pocket cost to you is $295, and Tempus offers payment plans.
You are not in this alone. We are here to help. Give us a call if you want more information or to complete pharmacogenomic testing.

